Diabetes is an incurable condition that affects blood sugar levels. According to the American Medical Association, one in twenty-five construction professionals has diabetes, and one in four is obese. Symptoms of type 2 diabetes include unexplained weight loss, frequent urination, dry eyes, and blurred vision. Luckily, there are steps you can take to prevent a diagnosis of type 2, including regular exercise, a healthier diet, and proper sleep.
Quick look
- There are three types of diabetes: type 1, type 2, and gestational.
- Symptoms of type 2 diabetes include unexplained weight loss, excessive thirst, and cuts and wounds that heal slowly.
- Overweight, inactive, and genetically predisposed people are most at risk for type 2 diabetes.
- Treatment for type 1 diabetes includes pills, insulin injections, and regular blood sugar monitoring.
- Type 2 diabetes isn’t reversible, but a healthy diet, regular exercise, proper sleep, and staying hydrated can help maintain blood sugar levels within a non-diabetic range.
Understanding diabetes

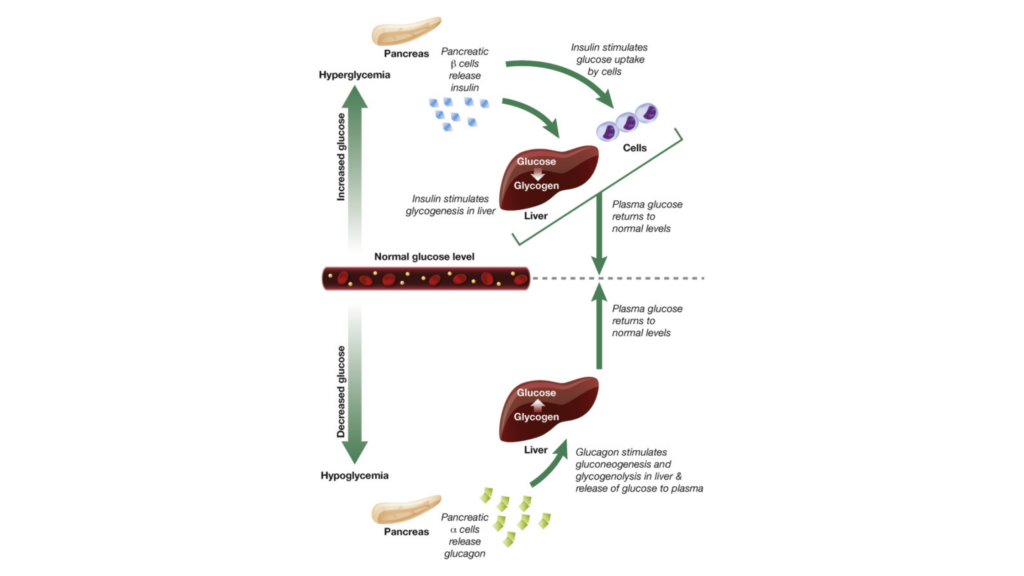
Diabetes is a lifelong disease that impacts how your body controls blood sugar (blood glucose). Glucose is your body’s primary energy source, and when levels are too high, it can affect various aspects of your health. Your body naturally produces some glucose, but the bulk of glucose comes from the diet.
People diagnosed with diabetes typically fall into one of two categories:
- Their bodies naturally don’t produce enough, and sometimes, no insulin
- The body doesn’t properly utilize insulin
Insulin, a hormone produced by the pancreas, shuttles glucose into cells, where it’s used for energy. However, if you have diabetes, the glucose remains in your blood, unable to reach your cells.
Diabetes puts people at a higher risk for some cancers, including breast cancer, pancreatic, colorectal, and bladder cancer. If not managed, it can lead to long-term damage to your kidneys, eyes, heart, and nerves. Taking steps to prevent diabetes could lower your risk for diabetes-related health conditions.
Types of Diabetes
Type 1
Type 1 diabetes is an autoimmune condition whereby your body destroys pancreatic β-cells, the cells responsible for producing insulin. As a result, your body makes little to no insulin, and it must be administered exogenously. Without sufficient insulin, type 1 diabetics can develop severe hyperglycemia and, ultimately, diabetic ketoacidosis, which can be fatal. Type 1 diabetes can develop at any age, although it’s often undiagnosed through childhood and young adulthood.
Type 2
There are typically two routes for type 2 diabetes: your body doesn’t produce enough insulin to maintain normal blood sugar levels, or your body doesn’t utilize insulin properly. As a result, too much glucose remains in the bloodstream and cannot reach cells. High blood sugar can lead to long-term health complications, such as circulatory, nervous, and immune system damage.
Type 2 diabetes is a more common diagnosis and typically develops in middle-aged people, but it can be diagnosed at any age. That said, lifestyle factors are hugely important with type 2 diabetes—if you implement a routine of a healthy diet and exercise, you could help delay or entirely prevent a diagnosis.
Gestational
Gestational diabetes is a type of diabetes specific to pregnancy. It affects how your body utilizes glucose, leading to high blood sugar levels, which pose a health risk for mom and baby. A blood test between weeks 24 and 28 will determine if you have gestational diabetes.
In most cases, blood sugar will return to normal after delivery, but having gestational diabetes increases the risk of getting type 2 diabetes.
Prediabetes
Prediabetes affects approximately 97.6 million, or 38% of the American adult population. You’re considered prediabetic when your blood glucose levels are abnormally high but not high enough to be considered type 2 diabetes. If you’re pre-diabetic, you have a higher risk of developing heart disease and diabetes in the future.
What is HbA1C?
The hemoglobin A1C test is a blood test used by health professionals to diagnose diabetes or help diabetic people understand the effectiveness of their treatment. It provides a snapshot of blood glucose levels within two or three months.
HbA1C test results are reported as a percentage, with the following results:
- 5.6% or lower: Normal
- 5.7-6.5%: Prediabetes
- 6.6% or higher: Diabetes
HbA1C is a helpful measure to gauge where your blood sugar levels are and what adjustments should be made to keep them within a normal range. Your healthcare provider will guide you on how often this test should be done, but a few times a year is standard if your treatments have been working and you haven’t been experiencing new symptoms. If your treatment results aren’t consistent, you may be asked to test more often. If you’re prediabetic or at risk of developing diabetes, it’s also essential to test as often as recommended by your doctor.
Who’s at risk for type 2 diabetes?
Certain factors increase the risk of developing type 2 diabetes—people who:
- Have a family history of diabetes
- Are overweight (including obesity)
- Are physically inactive
- Have prediabetes
- Have had gestational diabetes
- Have high blood pressure or high cholesterol
- Have certain pre-existing health conditions (NAFLD, PCOS, etc.)
- Are taking certain medications
- Are of certain ethnicities
Genetics and lifestyle factors both play a significant role in diabetes risk, so it’s essential to understand where you sit on the risk spectrum to determine the next steps.
Signs and symptoms of type 2 diabetes
When you have type 2 diabetes, some or all glucose stays in your blood and cannot go towards energy production. Here are some of the most common symptoms of type 2 diabetes:
- Frequent urination
- Unexplained weight loss
- Feeling very thirsty
- Recurring thrush or unexplained itchiness in the genital area
- Dry eye lenses and blurred vision
- Cuts and wounds that heal slowly
Diabetes diagnosis
If you suspect you may have diabetes, there are several methods for diagnosis.
- HbA1C: The hemoglobin A1C test is a blood test doctors use to diagnose diabetes or help diabetic people understand how well their treatment is working.
- The oral glucose tolerance test: Measures your body’s glucose levels in a fasted state after consuming a glucose drink. This test is most commonly done to check for gestational diabetes and typically takes between 1 and 3 hours.
- The random plasma glucose test: A measure of how much glucose is in your blood at any point (non-fasted).
- The fasting plasma glucose test: A measure of blood glucose in a fasted state. This most accurately represents a person’s baseline blood sugar levels.
A doctor may also look for other diabetes markers, such as autoantibodies, proteins, or genetics, to determine your type.
Diabetes treatment
The goal of both type 1 and type 2 diabetes treatment is to maintain glucose levels within a normal and healthy range. Here’s what treatment may look like for both types.
Type 1
Type 1 diabetics must administer insulin and check blood sugar levels multiple times daily through a glucose device or continuous glucose monitor (CGM). A CGM is a convenient way for busy professionals to monitor glucose levels without worrying about pricking their fingers every few hours.
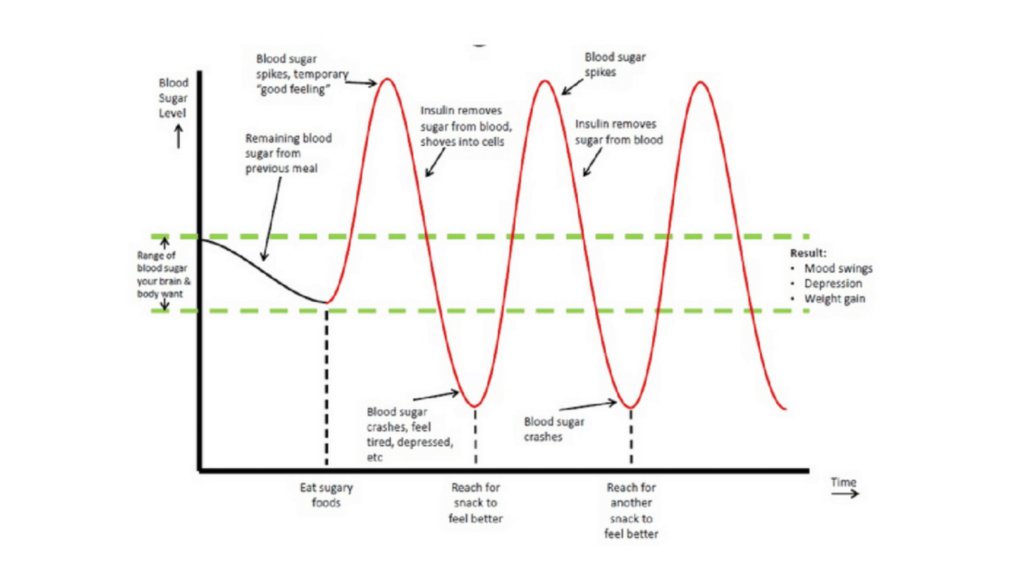
If blood sugar levels fall below the normal range, it can lead to hypoglycemia and symptoms like hunger, shakiness, and feeling faint. Consuming a sugar-rich meal or snack is the fastest way to increase blood sugar, but other options include glucose tablets, Glucojuice, or pure glucose if you need to treat the symptoms urgently. Hyperglycemia (high blood sugar) usually results from eating something too sugary or overeating. In that case, monitoring diet and making adjustments is the simplest fix.
In more extreme cases, type 1 diabetes can be treated with hypertensive medicines, low-dose aspirin, an angiotensin-converting enzyme (ACE) inhibitor, or in some cases, a pancreas transplant.
Type 2
Management of type 2 diabetes is primarily lifestyle-related. Proper diet and exercise can go a long way in managing blood sugar levels if you’re in the early stages. Still, depending on the severity, medication may be needed to support lifestyle changes. Aside from medicines via tablet, you may have to administer insulin via injection.
Tablet or pill options for type 2 diabetes include dapagliflozin, canagliflozin, empagliflozin, metformin, sulphonylureas, or Gliptins (DPP-4 inhibitors). If you test your blood sugar and you’re hypo or hyperglycemic, you can use similar dietary treatment options as people with type 1 diabetes.
Tips and tricks for managing diabetes

Any medication or recommendation from your doctor should be your first line of defense, but here are some ways you could also manage your diabetes.
1. Physical exercise
Exercise is integral to physical health, especially for those with diabetes. Not only will it help boost overall physical fitness, but exercise also helps control weight and stabilize blood sugar levels, reducing the risk of complications from diabetes. Strength training, biking, walking, and swimming are great options for routine workouts. For people who are not physically active, starting with gentle exercise is recommended.
2. Healthy diet
For people with diabetes, a low-sugar, lower-carb diet that focuses on whole foods is typically recommended. Meals should be consumed every 4-6 hours apart to avoid hyper- or hypoglycemia. Here are a few things to consider with your diet:
- Protein: Protein has minimal impact on blood sugar and should be included in every meal. Aim for about a fist’s size serving of high-quality proteins like beef, salmon, lamb, and poultry without the skin. Meatless options include black beans, peas, hummus, edamame, and nuts. Always boil, steam, or bake your protein choices over frying them.
- Complex carbs: Carbs impact blood sugar the most, so intake should be moderated. When choosing carbs, always choose complex carbs over simple ones to mitigate rapid blood sugar spikes. Sweet potatoes, rutabaga, turnip, quinoa, and other root vegetables are high-fiber options. Serving sizes vary based on age and weight but typically between 45 and 75 grams per meal.
- Healthy fats: Like protein, fats have minimal impact on blood sugar, making them a suitable addition to every meal. When consuming fats, limit/avoid industrial seed oils and unhealthy fats. Opt for things like avocado, almonds, flaxseed, olive or coconut oil, and natural nut butter, and always be sure to read nutritional labels for additives. Avoid trans fats where you can, and if you eat saturated fats like ice cream, egg yolk, cream cheese, and bacon, do so in small amounts.
- Low-glycemic fruits: Fruits are a concentrated source of carbohydrates and sugar. Because they can spike glucose quickly, choose low-glycemic fruits such as cherries, apples, grapefruit, apricots, strawberries, plums, and oranges.
3. Blood sugar monitoring
The average person with diabetes tests their blood sugar at least four times daily, but more frequent testing may sometimes be required. Traditional finger-prick tests are standard, but continuous glucose monitors provide an easy and instant result, especially during busy workdays. They also provide alerts when blood sugar levels are out of normal range. Knowing your blood sugar levels helps you understand which foods impact your glucose levels most and whether your body is leaning toward hypo or hyperglycemia.
4. Sleep
Sleep is crucial for blood sugar management, as it’s heavily involved in regulating metabolism. Getting adequate restorative sleep is also essential for managing glucose levels. Sleep deprivation, even partially over one night, can increase insulin resistance and blood sugar and, as a result, increase the risk of developing type 2 diabetes.
5. Hydration
Dehydration causes fluid levels in your blood to drop, concentrating and increasing sugar levels. Proper hydration is crucial to keeping blood sugar levels stable. Even mild dehydration can cause your blood sugar to fluctuate, typically causing hyperglycemia, because when you have less water in your bloodstream, your blood sugar concentration rises. Aim to consume 2-3L of water daily to maintain healthy hydration levels. Adding an electrolyte product to your water can also replace essential minerals that may be lost through urine or sweat.
6. Supplements
Supplements are also a great way to manage blood sugar. Here are a few to consider:
- Cinnamon: Cinnamon or supplements containing cinnamon have been shown to help reduce serum glucose, triglyceride, LDL cholesterol, and total cholesterol levels.
- Vitamin D: Vitamin D improves the function of pancreatic β-cells and boosts your body’s responsiveness to insulin.
- Magnesium: Low magnesium levels are typical in people with type 2 diabetes. Magnesium improves glucose metabolism and supports regular insulin action and secretion.
- Chromium: Chromium supports the activity of your pancreatic β-cells and helps regulate blood sugar levels.
Bottom line
Understanding the symptoms, knowing the risks, and routinely completing your annual physical exam could help you determine whether you have prediabetes or diabetes. For type 2 diabetes, in particular, lifestyle habits play a huge role in managing the disorder. Regular exercise for weight management, a healthy diet, adequate sleep, and proper hydration are all easy changes that can profoundly affect blood glucose levels.
If you are genetically predisposed to diabetes or you experience signs or symptoms, see a healthcare professional as soon as you can.
Like this article and want more like it? Subscribe to our weekly newsletter for the latest health and wellness tips and advice for people in the AEC space delivered directly to your inbox—it doesn’t get much more convenient than that.